More evidence surfaced this week that children continue to be the latest casualties of the Trump Administration. A new report shows that about 828,000 fewer children nationwide were enrolled in Medicaid and CHIP at the end of 2018 than in 2017.
That statistic is alarming because it could mean that the child uninsured rate – which has been steadily declining since the historic enactment of CHIP in 1997 under President Clinton – has reversed itself and is now on the rise. But we won’t know for certain until more survey data becomes available.
 Nonetheless, the new report, Medicaid and CHIP Enrollment Decline Suggests the Child Uninsured Rate May Rise Again, published by the Georgetown University Center for Children and Families, is disturbing. Although there are many reasons why fewer children are being served by Medicaid and CHIP (and some of those reasons are complicated), two stand out.
Nonetheless, the new report, Medicaid and CHIP Enrollment Decline Suggests the Child Uninsured Rate May Rise Again, published by the Georgetown University Center for Children and Families, is disturbing. Although there are many reasons why fewer children are being served by Medicaid and CHIP (and some of those reasons are complicated), two stand out.
First, as part of the 2017 GOP tax bill, passed by Congress and signed by President Trump, the individual mandate provision included in the Affordable Care Act was repealed. In addition, the Trump Administration has slashed funding for outreach and consumer assistance – programs aimed at educating particularly vulnerable populations about, for example, the availability of Medicaid expansion.
Second, as Voices for Human Needs has noted here and here, the Trump Administration’s immigration policies – including the proposed “Public Charge” rule that hasn’t even been implemented – have had a chilling effect on immigrant families who fear that accessing public benefit programs would threaten their future immigrant status and even put them at risk for deportation.
“The federal government took several steps that undermined enrollment including cutting outreach and consumer assistance funding to help families,” said Tricia Brooks, the lead author of the report. “Proposed immigration policies have kept many eligible families from seeking or renewing coverage for their children.”
There are other reasons for the decline in enrollment – among them are state hurdles and bureaucracy. Examples: Georgia shuts down its online application after normal business hours because of its inability to handle the extra volume of work due to limited staff. In Missouri, families report facing hours-long waits on the state’s phone lines to get help in enrolling or renewing coverage. Tennessee sent renewal packets to families that could be as long as 47 pages to verify their enrollment. And Texas is disenrolling more than 4,000 children monthly when it conducts income reviews for Medicaid at months 5, 6, 7, and 8 of enrollment. Children in families with more moderate incomes who are enrolled in CHIP are not subject to the same reviews.
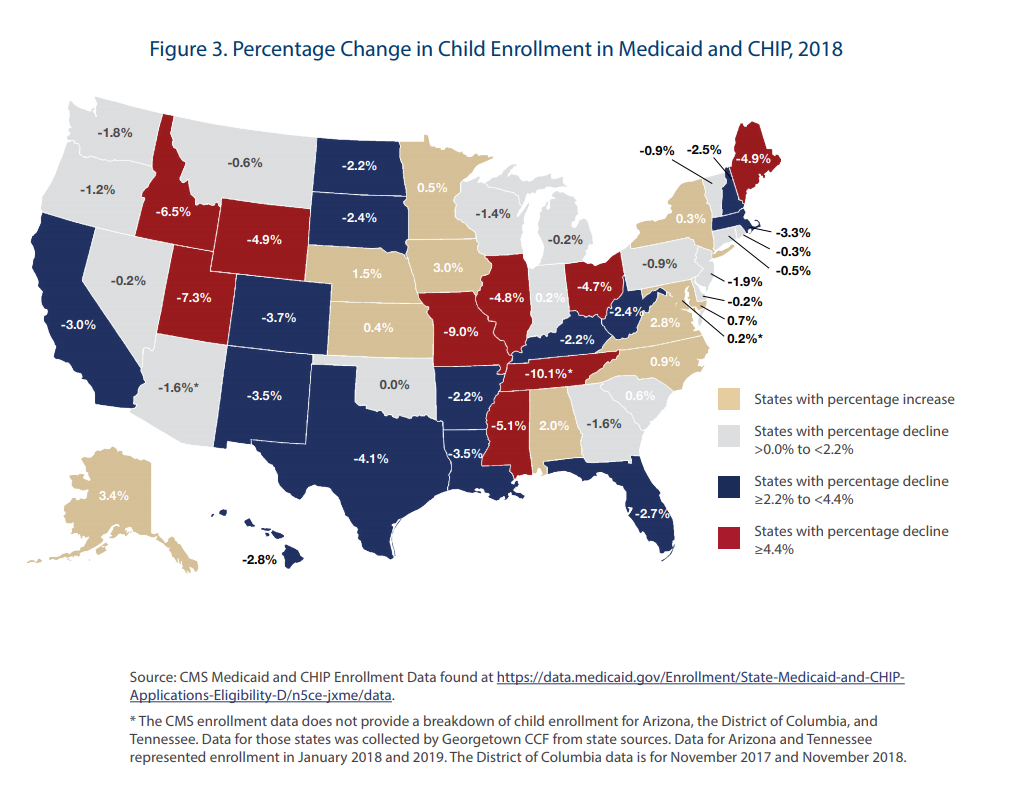
To put the numbers in context: between 2008 and 2016, the number of uninsured children in the U.S. dropped by more than half from 7.6 million to 3.6 million, achieving the milestone of coverage for more than 95 percent of U.S. children. Between 2000 and 2016, child enrollment in Medicaid/CHIP increased or held steady in all but one year. But from 2017 to 2018, the 828,000 fewer children enrolled in Medicaid/CHIP represented a significant 2.2 percent drop.
But numbers do not tell the whole story or properly frame the importance of providing children with good quality health care. As we’ve noted often in the past, and as the report reminds us, access to health care contributes to improved outcomes in early childhood, a critical time in brain development. The report notes that if children losing Medicaid/CHIP become uninsured, negative consequences include less access to primary and preventive care, increased exposure to medical debt, and longer-term educational and income impacts.
“This report puts federal and state policymakers on notice that the success the U.S. has achieved on children’s health coverage is in jeopardy,” said Joan Alker, Executive Director of the Georgetown University Center for Children and Families. “Federal and state leaders must acknowledge the problem, investigate its causes, and take immediate action to ensure children have the health coverage they need to succeed.”
At least some members of Congress are on notice. As we noted in the latest CHN Human Needs Report, on May 16, the House passed a measure that would, among other things, provide funding for states to establish state-based marketplaces under the Affordable Care Act and restore funding cuts by the Trump Administration for the ACA’s marketing and outreach, and for its navigator program, which helps people sign up for coverage.
Unfortunately, many health care advocates do not expect the Senate to take up the legislation and, in any case, the Trump Administration has threatened a veto.


The views and opinions expressed in this post are those of the author(s) and do not necessarily reflect those of MomsRising.org.
MomsRising.org strongly encourages our readers to post comments in response to blog posts. We value diversity of opinions and perspectives. Our goals for this space are to be educational, thought-provoking, and respectful. So we actively moderate comments and we reserve the right to edit or remove comments that undermine these goals. Thanks!